
Following publication of the NHS 10-year plan it’s increasingly clear that pharmacies will play a key role in the future model for Neighbourhood health services. As more pharmacists become independent prescribers there will be a growth in clinical services offered by pharmacies. This will include the assessment and treatment of a wider range of minor illnesses, chronic disease management and disease prevention.
As pharmacists embrace these changes, they will need to structure their patient consultations in a way that reduces clinical risk, maximises patient safety, allows seamless transfer of clinical information across medical professionals and allows them to work efficiently in an environment that is already time pressured.
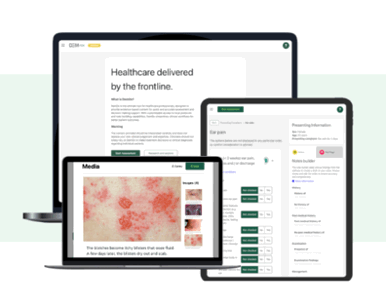
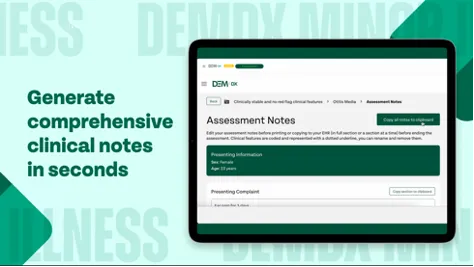
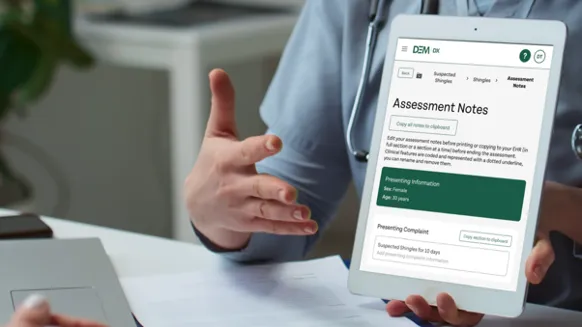
There are a number of software tools/apps designed to assist pharmacists to safely manage minor illness and injury consultations. One of the leaders in the field is DemDx, a clinical decision-making platform designed specifically for Pharmacists and Advanced Clinical Practitioners. This tool gives pharmacists confidence in their diagnostic decision making, streamlined safe consultations, evidence-based management plans and high-quality clinical notes.

All clinical consultations carry clinical risk, as the NHS 10-year plan encourages pharmacists to take on more primary care consultations, pharmacists will need to take proactive steps to manage these risks; both to protect patient safety and to protect the pharmacist’s professional licence and reputation.
There has been a steady increase in medical negligence claims across the NHS, Pharmacists are as vulnerable to medical litigation as other clinicians working in primary care. As such, a good framework of clinical governance is imperative to ensure pharmacy services are provided in a clinically safe, high-quality manner.
To reduce the risk of patient harm, complaints or medico-legal claims pharmacists should robustly identify and manage risks. Risk mitigation includes:
- Education and Training – all pharmacists consulting with patients must be able to evidence appropriate and up-to-date training, both in the clinical conditions they are managing and in wider topics such as Child and Adult Safeguarding.
- Policies and Procedures – every pharmacy should have clearly documented procedures (Standard Operating Procedures/SOPs) to manage all aspects of the patient pathway, including the appointment booking process, notes storage and sharing processes, referral processes and patient navigation pathways.
- Record keeping – the consulting pharmacist should make clear, detailed consultation notes at the time of the consultation and store them in a secure electronic health record. Good notes are critical to:
- Provide a concise account of the consultation and management plan.
- Ensure colleagues, including the patient’s GP, can readily see what’s happened, ensuring good continuity of care.
Clinical notes should follow the standard primary care consultation format, with the following as a minimum:
- Presenting Complaint – the main symptom that’s bringing them in today.
- History of presenting complaint – duration and severity of symptoms, description of the symptoms e.g. is pain heavy/tight/colicky/constant/intermittent, any associated symptoms, has the patient had similar problems in the past.
- Past medical history
- Drug History
- Family history – where relevant, e.g. in the wheezy child ask if parents/siblings have asthma.
- Social history – including smoking, drug and alcohol usage.
- Examination – include vital signs where possible e.g. temperature, pulse, BP and oxygen saturations and all examination findings including negatives, e.g. inflamed tonsils, no exudate.
- Likely diagnosis – this doesn’t have to be specific, e.g. sometimes it’s fine to say a child has a non-specific viral rash, as long as it’s been documented that more serious causes of rashes have been excluded.
- Management plan – including details of prescribed medication, over-the-counter meds, self-help advice, if follow up is needed and whether it has been arranged.
- Safety netting information – always include verbal advice on what symptoms/signs to be concerned about and when/how to seek medical advice. Document the safety net advice you have given and, where possible, back up your information with other patient resources, e.g. www.nhs.uk.
- Provide evidence should there be a complaint or investigation in the future.
When making notes remember “If it isn’t written down, it didn’t happen”, it’s not an acceptable defence for a clinician to say they did something because they always do. Pharmacists must document all key history and examination findings and that they’ve explored red flags to ensure a robust defence should the consultation lead to a complaint, claim or investigation.
- Red flags – Presence is as important as Absence! Asking the patient about the presence or absence of relevant red flags is vital to help clinicians safely reach the right diagnosis and to give medico-legal protection. For example, in every low back pain consultation ask the red flag questions and document their presence or absence, e.g. document the presence or absence of leg weakness/numbness, genital/buttock numbness, bladder or bowel difficulties, etc.
- Consultation Time and Interruptions – a busy pharmacist is likely to be multi-tasking and supporting junior team members. Clinical consultations with patients require dedicated time and space. Most GP consultations are moving from 10-minute to 15-minute slots; pharmacists should aim to offer a minimum of 10 minutes and ask staff not to disturb the consultation.
- Lack of access to the patient’s full medical record – unlike GPs and hospital clinicians, many pharmacists will be meeting the patient for the first time with no access to their medical history. Evidence suggests patient safety issues are more common when there is no access to the full medical record. Be conscious of this risk and always check with the patient or their carer if they have any significant medical history, e.g. immune suppression, diabetes, etc. It is surprising how often patients with high-risk medical histories, such as chemotherapy in the last few weeks, don’t mention it until asked!
- Continued professional development – pharmacists should only consult with patients that fall within their scope of practice. Patients should be navigated to another service if the patient’s presentation is outside their skill set. Medicine, like pharmacology, is lifelong learning with continual new and changing guidelines. Pharmacists should always practise in accordance with UK evidence-based guidelines. CKS NICE is an excellent resource, giving guidelines on diagnosing and managing most primary care presentations, all based on NICE or other approved national guidelines. Some consultation support tools, such as DemDx, base all their clinical content on NICE CKS, giving pharmacists assurance that their management is evidence-based.
To ensure pharmacy teams are practising safely they should consider instigating a rolling programme of clinical notes audit (GP consultation audit templates are available online). If audit results are low, develop an action plan for improvement and then re-audit in a few months. Always keep audit results for appraisals.
- Medical Indemnity – and finally, despite taking all the steps above there will still be times when consultations don’t end well. Pharmacists need financial protection against such situations. All consulting pharmacists and independent prescribers should have appropriate medical indemnity or insurance in place to protect against liabilities they might incur whilst practising. There is a lack of clear guidance on the level of cover needed but £10 million is often quoted.
Author:
Dr Sally Johson, GP MBBCh, MRCP (Paeds), MRCGP, DRCOG
Chief Medical Officer, DemDx

